An Introduction to the Role of Infant Massage in Neonatal Abstinence Syndrome (NAS)
An ever-growing problem in modern society and a significant global public health concern (Lee et. al. 2021), infants born to mothers who use drugs are at risk of adverse neonatal outcomes (Government of Western Australia Child and Adolescent Health Service, 2020; Casper 2014; Royal Women’s Hospital Victoria, 2018; Department for Health and Wellbeing, Government of South Australia, 2022; Sajadi et. al 2019). Neonatal abstinence syndrome (NAS) refers to the clinical picture of a collection of symptoms an infant may experience due to the withdrawal from in-utero substance exposure (MacMillan, 2019). The syndrome may occur as a result of maternal use of a variety of drugs, including opiates (heroin, buprenorphine, methadone and suboxone), amphetamines, alcohol and cocaine and its derivatives, as well as benzodiazepines (Government of Western Australia Child and Adolescent Health Service, 2020; Royal Women’s Hospital Victoria, 2018; Department for Health and Wellbeing, Government of South Australia, 2022). Abnormal neurobehaviours have also been reported in infants born of maternal use of marijuana, caffeine, volatile substances and new SSRI (serotonin reuptake inhibitor)/SNRI (serotonin and norepinephrine reuptake inhibitor) antidepressants (Royal Women’s Hospital Victoria, 2018; Department for Health and Wellbeing, Government of South Australia, 2022).
Environmental factors such as socioeconomic status and prenatal care of the infant play a substantial role in treatment and recovery of NAS. So much so, it is fundamental that parents receive continued support and education as they navigate their way through their parenting role and drug addiction (Anbalagan & Mendez 2023). To achieve this, care services must look for ways to provide a supportive environment and empowering tools for mothers to support their baby’s recovery, and their own, during their hospital stay and onwards.
In 2020, Pahl et. al undertook a systematic review of the Cochrane Library in order to assess whether non-pharmacological support practices were effective in improving important clinical outcomes including shortening hospital stays in opioid NAS cases. Reviewing only random controlled trials that examined the effect of a mechanical rocking bed, prone positioning, non-oscillating waterbed, and a low-stimulation nursery (Pahl et. al. 2020), unfortunately, their review fell short of including essential non-pharmacological care known to be effective, such the skin-to-skin contact afforded by kangaroo care, as well as nurturing infant massage.
The purpose of this report is to demonstrate not only the benefits of supplementing medicated and non-medicated treatment of NAS with infant massage, but also using infant massage to empower parents with bonding and ongoing care of their infant and relieving them of some stress and depressive symptoms, while somewhat alleviating NICU nurses of the negative effects of their experiences in dealing with these situations.
Figure 1: Infant Massage in the NICU
(Hanlon 2014)
Neonatal Abstinence Syndrome (NAS)
The symptoms of NAS are varied and significant. CNS hyperirritability may present as high-pitched crying, tremors, sleep disturbances and irritability; autonomic symptoms such as fever, frequent yawning, sneezing, sweating and/or mottling of the skin, as well as gastrointestinal disorders including excessive sucking, poor feeding, vomiting, loose/watery stools and posseting (regurgitation). Respiratory symptoms may also occur, including tachypnoea (rapid breathing), chest recession/retraction and nasal flaring (Government of Western Australia Child and Adolescent Health Service, 2020; Patrick et. al 2015). Infants exposed to cocaine have been found to develop sensory and motor delays, a reduced response to social stimulation and attention deficits (Arendt, Minnes & Singer 1996).
Negative long-term outcomes have also been documented in infants with prenatal opioid exposure (Anbalagan & Mendez 2023). Children born with NAS are two times more likely to develop attention-deficit/hyperactivity disorders, aggression and conduct disorders, anxiety, and adjustment disorders (Anbalagan & Mendez 2023). Additionally, their risk of being hospitalised for maltreatment, trauma, and behavioural problems is higher, while ‘mortality rates have been consistently higher among opioid-exposed infants for many decades and across many developed countries’ (Anbalagan & Mendez 2023, para. 41).
NAS Diagnosis & Conventional Treatment
While a reduction in the severity of symptoms and need for treatment has been observed in preterm opioid-NAS infants due to shorter exposure periods (Ruwanpathirana et. al. 2015), Armbruster et. al (2021, p. 107) state that although neonatal ‘opioid drug exposure is associated with an increased risk of preterm birth… [they] may not exhibit the same withdrawal symptoms as term infants diagnosed with neonatal abstinence syndrome (NAS)’. In cases of short-acting opioid exposure, these symptoms typically present in the infant’s first 24 hours after birth, while long-acting opioid exposure develops within the infant’s first 72-96 hours of life (MacMillan, 2019). Although it is not currently possible to predict if an infant will develop NAS prior to birth (Royal Women’s Hospital Victoria, 2018), accurate diagnosis involves a maternal history of substance use in conjunction with postnatal clinical observations using the Finnegan Scoring System (Government of Western Australia Child and Adolescent Health Service, 2020) up to five days after birth (Royal Women’s Hospital Victoria, 2018).
Depending on the severity of symptoms, treatment may involve the administration of medications. Morphine may be used in opiate withdrawal and Clonidine and/or Phenobarbitone as an adjunct to morphine or as a primary medication in cases of non-opiate withdrawal, with research showing that a stringent weaning regime plays a role in advancing recovery rates (Government of Western Australia Child and Adolescent Health Service, 2020).
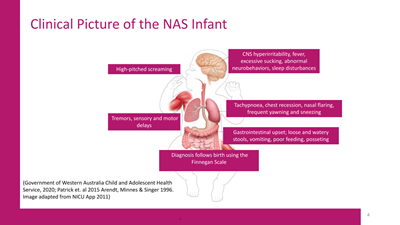
Figure 2: Neonatal Abstinence Syndrome
(Adapted from NICU App 2011)
Non-pharmacological treatment heavily involves parental education and participation, and includes supportive therapy such as cuddling, skin-to-skin contact, rooming-in, swaddling, the use of pacifiers/mittens, regular quiet, reassuring and soft talk to the infant, the use of comfortable bedding (ie: sheepskin underneath cot sheet) with adequate ventilation and small frequent feeds on demand, in a quiet environment with reduced stimulation. Infants may also be winded regularly while nappies are changed and barrier cream applied after every feed. (Royal Women’s Hospital Victoria, 2018; Government of Western Australia Child and Adolescent Health Service, 2020; Department for Health and Wellbeing, Government of South Australia, 2022).
Due to its multitude of benefits, breastfeeding is often recommended in NAS. Although studies surrounding breastfeeding and NAS are limited, Yen & Davis (2022), it is important to note that concentrations of opioids buprenorphine and methadone in breastmilk analyses ‘are low and pose minimal risks to neonates’ (Yen & Davis 2022, pp. 2). Yen and Davis (2022) also mention that the benefits of breastfeeding the infant with opioid NAS include less severe withdrawal symptoms, shorter hospital stays and a decrease in the need for pharmacological intervention. Further, the Royal Women’s Hospital Victoria (2018) recommend breastfeeding in cases of NAS, as long as the mother isn’t using heroin, crystal methamphetamine, is on any drugs other than methadone, buprenorphine or suboxone, or is HIV positive.
The Benefits of Infant Massage for the NAS Baby
One of the oldest and effective healing modalities in the world, massage is known for its ability to promote calm, growth and reduce pain in adults, children and infants alike (Gholami et al 2021). A beautifully healing modality, infant massage involves specialised techniques that soothe, calm and nurture the baby while cultivating healthy bonds between mother and child.
Interestingly (and somewhat sadly), other than a supplement to first-line treatment in South Australia (Department for Health and Wellbeing, Government of South Australia, 2022), infant massage does not appear to be indicated in any other clinical or governmental non-pharmacological guidelines for the intervention of NAS in Australia. This is despite the fact that infant massage has been shown to improve respiratory function, immune and gastrointestinal function, reduces jaundice, calm and nurture the nervous system while alleviating pain, improving growth outcomes in preterm infants and encourage neurodevelopment (Lesarti et al 2021; Adbellatif et al 2020; Fitri et al 2021; Pados & McGlothen-Bell 2019; Badr et al 2015; Gholami et al 2021; Maguire 2014; Hahn et. al. 2016).
Moreover, at an estimated lifetime cost exceeding USD 100,000 per year, per NAS-diagnosed child, rising healthcare costs and limited resources, exploring non-pharmacological methods of improving symptoms and health outcomes has become a point of necessity (Lee etl. Al 2021). Karimi et. al (2021) concurs, advocating complementary modalities including infant massage, as they are economical, have no serious adverse effects, drug reactions or interactions, and they are easy to carry out.
In 2014, Maguire noted that there were no published studies regarding the impact of infant massage specifically on neonates suffering from NAS (Maguire 2014), however, perhaps due to a contemporary surge in prevalence (Lee et. al. 2021), the subject appears to have ignited an interest within the medical community and studies are slowly but surely being undertaken. Determined to improve upon existing research on non-pharmacological interventions for NAS, the most prominent qualitative study surrounding infant massage for NAS specifically was published in 2016 by Hahn et. al. The authors sought to further their understanding of how infant massage could impact the infant’s behavior and the mother’s relationship with their infant through a series of two interviews: one in-person following the infant massage education session, and the other two weeks post-discharge. From a total of eight mother-infant pairs, the authors found that NAS infants were calmed and comforted by infant massage; their sleep and feeding improved, and crying was reduced. The authors also added that the skin-to-skin contact elicited during infant massage demonstrated a decrease in pain scores, and it significantly facilitated the mother-child bond (Hahn et. al. 2016). Although limited by its small sample size and qualitative design, the paper is a major step forward in the accumulation of evidence supporting infant massage for infants suffering NAS.
.png?width=399&height=266)
Figure 3: NAS baby in the NICU
(Nashville Medical News 2019)
Also, foot reflexology, which is performed during an infant massage in small quantities, was studied in 31 neonates with NAS based in Iran (Sajadi et. al 2019). In this recent 2019 modified double blind clinical trial, the maternally used drugs involved 71% opium and its derivatives 19.3% methadone and 9.7% heroine. The infants, who remained on any prescribed pharmacological treatment throughout the study, received 15 minutes of foot reflexology on the first horizontal zone twice a day. Their findings were significant; NAS symptoms as measured before and 20 minutes after intervention, were considerably improved. Although they have not specified exactly which NAS symptoms were successfully improved, the authors hypothesised that the impact of the foot reflexology intervention, which incorporated the sole of the foot and the toes, corresponded with areas that are related to the head, neck and opioid production in the body. Interestingly, the foot reflexology intervention triggered meconium excretion in 41.9% of infants (Sajadi et. al 2019), suggesting a probable positive impact on the digestive system. An appendix comprising the actual reflexology massage strokes and points would have been a highly valued addition to the paper, however it is an excellent contribution to the accumulating evidence of infant massage in NAS.
In light of the fact that 20-40% of opioid-NAS infants are premature (Allocco et. al 2016), and that infants admitted to NICU’s are often exposed to a range of painful interventions (Gholami et al 2021), further exploration is warranted to better understand the role of infant massage in pain relief of premature neonates.
A 2021 study of premature infants admitted to the NICU sought to assess the impact infant massage and kangaroo care on pain scores of neonates (Gholami et al 2021). Pain scores were assessed via the Neonatal Pain Scale, which measures intensity of crying, facial expressions, breathing patterns extremity movement and level of consciousness. For 5 minutes, three times a day until the end of their stay in the NICU, mothers massaged their babies in a prone position, working from head to toe. The study found that both infant massage and kangaroo care significantly reduced neonatal pain scores (Gholami et al 2021).
The results of this study correlate with a similar study by Karimi et. al 2021. In their double-blinded three-group clinical trial that aimed to compare the effects of kangaroo care and preterm infant massage on pain scores. Infants in the NICU received three 5-minute massages from protocol-trained licenced massage therapists, for five consecutive days. Using the Neonatal Infant Pain Scale to assess neonatal pain scores, they found that infant massage significantly reduced pain in preterm infants and concluded that this was due to the acceleration of their neurobehavioral development and the maturation of the autonomic nervous system. (Karimi et. al. 2021).
Given the nature of drug treatment and subsequent elimination, liver health is a serious consideration for NAS infant treatment and health outcomes and is routinely monitored during hospitalisation. The general readmission of infants with NAS, which can occur up to one year following initial discharge, varies from 3-4% depending on whether the baby was preterm or experienced NAS-resultant complications (Patrick et. al. 2015). However, in their research article, Patrick et. al (2015) found that ‘jaundice was the most frequent primary diagnosis for both late preterm infants (34.5%) and uncomplicated term infants (51.2%)’ with NAS (Partrick et. al. 2015, pp. 515).
In a review and network meta-analysis of randomised controlled trials using infant massage and phototherapy in neonatal jaundice, Abdellatif et. al (2020) concluded that although phototherapy was still required, infant massage may be an effective adjunct to phototherapy to reduce phototherapy duration for jaundice. These are promising results, however further NAS-specific investigations are indicated.
Of some significance with respect to incidences of jaundice in NAS, back in 1972 it was found that infants born to heroin-addicted mothers exhibit ‘a lack of significant jaundice, suggesting a possible mitigating effect of heroin on bilirubin accumulation in the newborn infant’ (Nathenson et. al. 1972, p. 899). While not much in the way of further studies have looked closely at these findings, it is interesting to note the impact that heroin has on the neonatal liver, and this may change treatment protocols.
Although some of these studies were not based around NAS, they could be used as a basis of rationale for further research into using infant massage to alleviate pain, discomfort and improve liver function for infants diagnosed with NAS.
Infant Massage, the Mother and NAS Recovery
Midtsund, Litland and Hjalmuhult (2018) argue that ‘awareness of maternal psychological emotions postpartum, when the mother is vulnerable, can be considered as essential when it comes to mother-child communication and connection’ (Midtsund, Litland & Hjalmuhult 2018, pp. 497).
Substance abuse often stems from a myriad of negative life experiences such as domestic violence and sexual abuse, leading to mothers who are susceptible to mental health issues including depression, low self-esteem, parenting stress and problems with maternal attachment (Porter et. al. 2015). Given the circumstances, it is known that drug-addicted mothers struggle to bond with their infants and can feel somewhat helpless in the recovery process (Anbalagan & Mendez 2023)
. Transitioning to parenting can be a struggle and create insecurity and stress (Midtsund, Litland & Hjalmuhult 2018) even in healthy populations, let alone mothers who are struggling emotionally and tackling substance abuse.
Parents are encouraged to be involved in their NAS infant’s recovery (Government of Western Australia Child and Adolescent Health Service, 2020). However, because more than 50% of mother’s engaging in illicit drug use have a co-existing psychiatric morbidity, most commonly depression (Department for Health and Wellbeing, Government of South Australia, 2022), it is essential mothers get the care they require for as long as needed.
Close and consistent contact with community support structures have been shown to positively impact the mother and infant, enriching the home environment to allow for the normal development of the infant (Anbalagan & Mendez 2023). In this highly complex and vulnerable population, ongoing postnatal support from NAS-educated health professionals such as paediatricians, social workers, child health nurses and social health organisations (drug and alcohol services) are vital to recovery and aftercare (Royal Women’s Hospital Victoria, 2018; Government of Western Australia Child and Adolescent Health Service, 2020; Department for Health and Wellbeing, Government of South Australia, 2022; Anbalagan & Mendez 2023).
Because touch is the very first sensory stimuli that forms the foundation of the initial relationship between a mother and her baby, massage therapy is one of the most central ways of emotional exchange between the mother-child dyad (Gholami et al 2021). Further, babies in the NICU may are frequently separated from their mothers, causing distress to both the mother and the infant (MacMillan 2019). Naturally, the mother is a pivotal participant in the treatment and recovery of both herself and her baby (Royal Women’s Hospital Victoria, 2018; Department for Health and Wellbeing, Government of South Australia, 2022). Any stay in the NICU is a stressful one for both the parents and their babies - their overall adjustment, wellbeing and attachment is significantly affected by how the mother copes with the NICU experience (Karimi et. al. 2021).
In the aforementioned study by Hahn et. al. 2016, the authors gathered evidence directly from a sample of these mothers in an effort to understand how infant massage impacted them as mothers with infants suffering NAS. They found that infant massage not only improved maternal empowerment, but also significantly enhanced mother-baby bonding, and brought about a sense of enjoyment. Playing a role in allaying feelings of guilt, mothers expressed positive attitudes towards being able to contribute to their baby’s recovery and enjoyed being involved in their ongoing care (Hahn et al 2016).
.
.png?width=399&height=266)
Figure 4: Mother with her NAS Baby
(May 2019)
An important study exploring the effect of a blended infant massage and parenting enhancement program on maternal psychosocial health outcomes was published in 2015 (Porter et. al, 2015). The authors aimed their study specifically at maternal-infant interactions between substance-addicted mothers (SAMs) and their infants participating in outpatient rehabilitation. In the three-month randomized, controlled, three arm experimental designed study, 138 mother-infant pairs were divided into two levels of psychoeducational intervention; those who received infant massage as well as an educational curriculum (IMPEP) and those who only participated in the educational curriculum (PEP); and a control group which did not participate in either, but continued usual care from respective support agencies. The IMPEP group undertook 4-weekly 2-hour classes. Using both objective and subjective measurement tools, the authors found a decrease in parenting stress and maternal depressive symptoms in the IMPEP group. While unable to demonstrate an improvement of self-esteem, mother attachment and mother-infant interaction during the course of the study, they note they cannot rule out the possibility of such interventions maintaining these elements over time (Porter et. al. 2015). Although they note that the classes were ‘taught by certified nurse practitioners and incorporated both demonstration and supervised practice of infant massage techniques, integrative group discussions as well as question-and-answer periods focused on childcare practices’ (Porter et. al. 2015, p. 319), it is not noted if the nurse practitioners were specifically trained in dealing with substance-abuse mothers, or infants with NAS. Further, infant massage methodology was not discussed in the paper.
In the same study by Gholami et. al (2021) that demonstrated a role for infant massage in neonatal pain reduction, the authors found that infant massage also assisted in effectively reducing maternal anxiety in otherwise healthy subjects. Following the infant’s admission and stabilisation in the NICU, mothers were trained in infant massage, and carried out five-minute sessions with their infants, three times a day; one hour after morning feeding, half an hour after mid-day feeding and 45 minutes after the second massage, until the end of their stay in the NICU. Anxiety levels were assessed using the Spielberger standard of overt and covert anxiety before and after the intervention. They found that by undertaking infant massage with their babies, positive feelings were cultivated to the point where her mental state level of anxiety was significantly reduced (Gholami et al 2021).
Consistent with these findings, the McCarty et. al. (2019) review also concluded that maternally administered infant massage ‘benefits mothers of preterm infants by reducing anxiety, stress, and depressive symptoms and improving maternal-infant interactions in the short-term’ (McCarty et. al 2019, p. 1).
Moreover, in addition to infant pain scores, Karimi et. al’s (2021) study also sought to determine the effects of kangaroo care and infant massage on stress, anxiety, depression and stress coping strategies on 90 mothers with preterm babies admitted to the NICU. Assessment tools including the Coping Responses Inventory for Adults (CRI-A), the Depression, Anxiety and Stress Scale (DASS-21) were utilised to measure outcomes. Although the mothers did not participate in the massage of their infant in this instance, the study found that anxiety, depression and stress was significantly reduced, and there was an increase in the understanding of strategies to deal with stress for the mothers (Karimi et. al 2021).
.
.png?width=400&height=266)
Figure 5: NAS Infant Massage
(NTMC 2023)
Midtsund, Litland and Hjalmuhult (2019) sought to investigate the effect of participation in infant massage training with mothers who were experiencing emotional challenges and stress in motherhood. Although it revolved around otherwise healthy subjects, their qualitative study of 12 mothers in Norway found that mothers welcomed the opportunity for emotional and physical connection with their babies – it provided feelings with confidence and an improved sense of self esteem as discovered new experiences regarding their baby’s presence. As a result of learning infant massage, they felt a deeper connection with their baby (Midtsund, Litland and Hjalmuhult 2019)
Again, although not NAS-based, these studies focused on non-pharmacological interventions such as infant massage for the benefit of the postnatal mother and her mental health. The articles are a positive illustration of the impact of infant massage on the mother’s emotional wellbeing and may not only serve as a valuable insight into the possible avenue of relief for the mother, but they also highlight the intricacy of the mother-child dyad and are also steppingstones for further research into using infant massage as a tool for improving mothers’ wellbeing in cases of drug use and infants with NAS.
Infant Massage and the NICU Professional Care Team
Caring for the health professionals involved in the treatment and recovery of mother and child in cases of NAS is an important consideration. Casper (2014) found that that neonatal NICU nurses ‘spend a significant amount of time caring for infants with NAS, but recent evidence indicates that nurses often lack the required knowledge to provide optimal care to the maternal-infant dyad’ (Casper 2014, pp. 377). NICU nurses also often experience a range of negative emotions surrounding maternal drug use and the subsequent impact on the infant during their hospital stay (Casper 2014).
Further to this, McCarty et. al (2023) note in their review paper that due to apprehension surrounding the maintenance of workload capacity, discerning infant medical fragility and the time it can take to learn infant cues, some NICU’s have been slow to incorporate infant massage into their regular standard of care. These are plausible concerns, especially considering the physiological and psychosocial vulnerability of the mother-infant dyad in cases of NAS, and the minimal quantity of NAS-specific infant massage studies. However, as McCarty et. al (2023) argues, once willing parents are trained in infant massage by a professional, the intervention could be provided by the parent simply with oversight from a member of the medical team. Additionally, NICU volunteers that hold infants when the mother is unable to be present (Maguire 2014) could also be trained in giving infant massage to the NAS baby, relieving medical staff workloads.
Somewhat allaying the concerns regarding the mental health of NICU nurses when dealing with NAS, Isaksson, Hedov and Garmy (2022), sought out childcare nurses’ experiences in teaching infant massage to parent groups. Although not NAS-based, throughout the qualitative, interview-based study, nurses expressed valuable observations that lead to the authors concluding that infant massage promotes attachment between parents/guardians and their infants, has a calming impact, and improves the parent/guardian relationship with their infants (Isaksson et. al. 2022).
As experts recommend non-pharmacological interventions in conjunction with necessary pharmacological treatment (Casper 2014), it stands to reason that empowering nurses with the skills to teach parents how to massage their babies - not only to draw upon the positive effects this brings about for both mother and child, but to provide a partial solution for nurses who are otherwise powerless over the situation - may result in more positive outcomes for all. Although this study was not based around settings of maternal drug addiction or NAS, however it represents an important basis from which further studies can be based, in an effort to further empower relevant health professionals dealing with these complex situations.
.
Figure 6: Infant Massage of the Preterm Baby
(Massage Magazine, 2017)
Frequently Asked Questions
How does infant massage benefit the NAS baby?
.
- Calm and comfort
- Sleep improvements
- Feeding, digestion improvements
- Mother-infant bonding
- Reduction in crying
- Reduction in pain scores
- Possible improvement of liver function/reduction in jaundice
What impact is there on the mother?
- Opportunity to contribute to infant recovery and comfort
- Empowering parental skills
- Mother-child bonding
- Possible decrease in anxiety, parental stress and depressive symptoms
Which massage oils should be used with the NAS baby?
.
- Not one study mentioned which type of massage oil was used for infant massage in NAS, however the IMIS direction of using natural, non-scented, plant-based, organic, cold pressed ingestible vegetable oils such as sesame oil, sweet almond oil or apricot oil is sound rationale; avoiding potential reactions while being nutritive to delicate skin, providing an appropriate lubricated medium and enabling the mother’s scent to be present throughout the massage.
One of the symptoms of the NAS baby is high-pitched screaming. How is permission from the infant sought in these cases?
.
- This aspect was not explored or detailed by any relevant studies, however, dealing with these cases much like cases of IMIS set procedure for colic provides for a pragmatic approach; comprising the calming, soothing voice of reassurance that a massage is about to begin.
What are the contraindications in massaging a NAS baby?
In cases of NAS, medical fragility is a concern especially if the infant is preterm, and medical clearance is essential. Close monitoring of cues during the massage will also ensure safety and efficacy, however, regular contraindications as stipulated by the IMIS (2017, pp. 40) still apply:
.
- Skin infections and bruising
- Cuts, abrasions, burns including sunburn
- Undiagnosed pain or masses
- Cardiovascular conditions,
- Thrombosis or embolism
What about pressure on medical staff to carry out/teach parent’s infant massage?
Developing a close working relationship with an IMIS certified Infant Massage Instructor and employing them to teach Infant Massage to parents directly eliminates concerns regarding workload capacity, however this needs to the weighed against the benefits for setting time aside for medical staff to be trained and to teach parents, as it is a potential partial solution for nurses who are otherwise powerless over the very complex situation of maternal drug addiction and NAS.
What are the impacts of infant massage and NAS on society as a whole?
Infant massage is an easy and cost-effective way of improving NAS recovery outcomes. While some studies advocate for infant massage as a safe, easy and cost-effective intervention that may reduce hospital stay duration, further studies focused on NAS-specific infant massage and its socioeconomic impact are needed.
Ancient Wisdom for a Modern Application
Although studies focused on the role of infant massage and NAS recovery for the mother-infant dyad are limited, there are clear indications that implementing infant massage into routine non-pharmacological care in cases of NAS are beneficial for both mother and child. Even though further research is essential to provide the evidence required for best practice, the plethora of positive health outcomes that arise from infant massage, demonstrates that infant massage is an economically viable, easy, safe and effective intervention for lessening the severity of symptoms in the NAS infant.
References
Abdellatif M, Vuong N, Tawfik G, Elfaituri M, Mansour M, Zaki M, Duong P, El-Qushayri A, Liang Y & Liu K, 2020, ‘Massage therapy for the treatment of neonatal jaundice: A systematic review and network meta-analysis’.
Journal of Neonatal Nursing, 26(1), 17–24
https://doi.org/10.1016/j.jnn.2019.09.002
Allocco E, Melker M, Rojas-Miguez F, Bradley C, Hahn K & Wachman E, 2016, ‘Comparison of neonatal abstinence syndrome manifestations in preterm versus term opioid-exposed infants’,
Adv Neonatal Care. 2016 October; 16(5): 329–336. DOI:10.1097/ANC.0000000000000320
Anbalagan S, Mendez M 2023, ‘Neonatal Abstinence Syndrome’, NCBI Bookshelf. National Institute of Health. Jan-April 29, 2023, available at
https://www.ncbi.nlm.nih.gov/books/NBK551498/?report=printable
Arendt R, Minnes S & Singer L, 1996 ‘Fetal Cocaine Exposure: Neurologic Effects and Sensory-Motor Delays’,
Phys Occup Ther Pediatr. 1996 January; 16(1-2): 129–144. DOI:10.1080/J006v16n01_09
Armbruster D, Schwirian, C, Mosier A, Tam W, Prusakov P, 2021, ‘Neonatal Abstinence Syndrome and Preterm Infants: A Look at Current Practice’,
Advances in Neonatal Care 21(2): p 107-114, April 2021. DOI: 10.1097/ANC.0000000000000858
Badr L, Abdallah B & Kahale L, 2015, ‘A Meta-Analysis of Preterm Infant Massage: An Ancient Practice With Contemporary Applications’,
The American Journal of Maternal/Child Nursing 40(6):p 344-358, November/December 2015. DOI: 10.1097/NMC.0000000000000177
Casper T, 2014, ‘Evidence-Based Nurse-Driven Interventions for the Care of Newborns with Neonatal Abstinence Syndrome’,
National Association of Neonatal Nurses, Vol. 14, No. 6 DOI: 10.1097/ANC.0000000000000118
Department for Health and Wellbeing, Government of South Australia, 2022, South Australian Perinatal Practice Guideline Neonatal Abstinence Syndrome (NAS),
Department for Health and Wellbeing, Government of South Australia, available via
https://www.sahealth.sa.gov.au/wps/wcm/connect/8f6387004ee4a47a858c8dd150ce4f37/Neonatal+Abstinence+Syndrome_PPG_V4_0.pdf?MOD=AJPERES&CACHEID=ROOTWORKSPACE-8f6387004ee4a47a858c8dd150ce4f37-ocQX8iX
Fitri S, Nasution S, Nurhidayah I & Maryam N, 2021, ‘Massage therapy as a non-pharmacological analgesia for procedural pain in neonates: A scoping review.
Complementary Therapies in Medicine, 59, 102735, available via
https://doi.org/10.1016/j. ctim.2021.102735
Gholami A, Karimi F, Ghasempour Z, Abolhassani M, & Rabiee N, 2021, ‘Comparison of the effect of kangaroo care and infant massage on the level of maternal anxiety and neonatal pain’,
Journal of Babol University of Medical Sciences, 23(1), 90–97. DOI
10.22088/jbums.23.1.90
Government of Western Australia Child and Adolescent Health Service, 2020, Clinical Guideline for Neonatal Abstinence Syndrome,
Government of Western Australia Child and Adolescent Health Service, available via
https://www.cahs.health.wa.gov.au/-/media/HSPs/CAHS/Documents/Health-Professionals/Neonatology-guidelines/Neonatal-Abstinence-Syndrome.pdf
IMIS 2017,
Infant Massage Training Manual and Student Handbook for Correspondence Study, Infant Massage Information Service: Heidi McLoughlin, Dural NSW Australia
Isaksson J, Hedov G & Garmy P, 2022, ‘Lessons learned from child health care nurses' experiences of teaching infant massage groups: A qualitative interview-based study’,
Nursing Open. 2023;10:2638–2647. DOI: 10.1002/nop2.1524
Hahn J, Lengerich A, Byrd R, BSN, Stoltz R, Hench J, Byrd S & Ford C 2016, ‘Neonatal Abstinence Syndrome: The Experience of Infant Massage’,
Creative Nursing, Volume 22, Issue 1, 2016, available via http://dx.doi.org/10.1891/1078-4535.22.1.45
Jazayeri Z, Sajadi M, Dalvand H & Zolfaghari M, 2021, ‘Comparison of the effect of foot reflexology and body massage on physiological indicators and bilirubin levels in neonates under phototherapy’,
Complementary Therapies in Medicine, 59, 102684, available via https://doi. org/10.1016/j.ctim.2021.102684
Karimi F, Abolhassani M, ghasempour Z, Gholami A & Rabiee N, 2021, ‘Comparing the effect of kangaroo mother care and massage on preterm infant pain score, stress, anxiety, depression, and stress coping strategies of their mothers’,
Int J Pediatr 2021; 9(10): 14508-14519. DOI: 10.22038/IJP.2020.500004.3990
Lee E, Schofield D, Azim S & Oei J, 2021, ‘Economic Evaluation of Interventions for Treatment of Neonatal Opioid Withdrawal Syndrome: A Review’,
Children 2021, 8, 534, available via https://doi.org/10.3390/ children 8070534
Lestari K, Nurbadlina F, Wagiyo W & Jauhar, M, 2021, ‘The effectiveness of baby massage in increasing infant's body weight’,
Journal of Public Health Research, 10(s1), 1–5, available via https://doi. org/10.4081/jphr.2021.2332
MacMillan K, 2019, ‘Neonatal Abstinence Syndrome - Review of Epidemiology, Care Models, and Current Understanding of Outcomes’,
Clin Perinatol 46 (2019) 817–832, available via
https://www.sciencedirect.com/science/article/abs/pii/S0095510819301009?via%3Dihub
Maguire D, 2014, ‘Care of the Infant with Neonatal Abstinence Syndrome Strength of the Evidence’,
J Perinat Neonat Nurs Volume 28 Number 3, 204–211
DOI: 10.1097/JPN.0000000000000042
McCarty D, Willett S, Kimmel M & Dusing S, 2023, ‘Benefits of maternally-administered infant massage for mothers of hospitalized preterm infants: a scoping review’, Maternal Health,
Neonatology and Perinatology (2023) 9:6, available via
https://doi.org/10.1186/s40748-023-00151-7
Midtsund A, Litland A & Hjalmuhult E, 2019, ‘Mothers experiences learning and performing infant massage – a qualitative study’, Journal of Clinical Nursing. 2019; 28: 489-498.
DOI: 10.1111/jocn.14634
Nathenson G, Cohen M, Litt I, & McNamara H, 1972, ‘The effect of maternal heroin addiction on neonatal jaundice’
The Journal of Pediatrics, 81(5), 899–903. DOI:10.1016/s0022-3476(72)80540-7
Pados B, & McGlothen-Bell K, 2019, ‘Benefits of infant massage for infants and parents in the NICU’,
Nursing for Women's Health, 23(3), 265–271, available via
https://doi.org/10.1016/j.nwh.2019.03.004
Pahl A, Young L, Buus-Frank ME, Marcellus L, Soll R, 2020, ‘Non-pharmacological care for opioid withdrawal in newborns (Review)’,
Cochrane Library Cochrane Database of Systematic Reviews, available via
https://doi.org/10.1002/14651858.CD013217.pub2
Partick S, Burke J, Biel T, Auger K, Goyal N & Cooper W 2015, ‘Risk of Hospital Readmission Among Infants With Neonatal Abstinence Syndrome’,
Hospital Pediatrics Volume 5, Issue 10, October 2015. DOI:10.1542/hpeds.2015-0024
Porter L, Porter B, McCoy V, Bango-Sanchez, Kissel B, Williams M & Nunnewar S, 2015, ‘Blended Infant Massage-Parenting Enhancement Program on Recovering Substance-Abusing Mothers' Parenting Stress, Self-Esteem, Depression, Maternal Attachment, and Mother-Infant Interaction’,
Asian Nursing Research 9 (2015) 318-327, available via http://dx.doi.org/10.1016/j.anr.2015.09.002
Ruwanpathirana R, Abdel-Latif M, Burns L, Chen J, Craig J, Craig F, Lui K & Oei J, 2015, ‘Prematurity reduces the severity and need for treatment of neonatal abstinence syndrome’,
Foundation Acta Pædiatrica. Published by John Wiley & Sons Ltd 2015 104, pp. e188–e194. DOI:10.1111/apa.12910
Royal Women’s Hospital Victoria, 2016, Neonatal Abstinence Syndrome (NAS),
Royal Women’s Hospital Victoria, available via
https://www.thewomens.org.au/images/uploads/fact-sheets/YAYB-Neonatal-Abstinence-Syndrome-2018.pdf
Sajadi A, Kazemi M, Bakhtar B & Ostadebrahimi H, 2019, ‘Comparing the effects of auricular seed acupressure and foot reflexology on neonatal abstinence syndrome: A modified double blind clinical trial’,
Complementary Therapies in Clinical Practice, Volume 36, August 2019, Pages 72-76, available via
https://doi.org/10.1016/j.ctcp.2019.06.002
Yen E & Davis J, 2022, ‘The immediate and long-term effects of prenatal opioid exposure’,
Front. Pediatr., 07 November 2022 Sec. Neonatology Volume 10 – 2022, available via https://doi.org/10.3389/fped.2022.1039055
Images
Cover Image: Hassan C, 2023, New approach gets newborns with opioid withdrawal out of the hospital sooner and with less medication’,
The Philadelphia Tribune, available at
https://www.phillytrib.com/news/health/new-approach-gets-newborns-with-opioid-withdrawal-out-of-the-hospital-sooner-and-with-less/article_0c65d790-a9e4-52f4-8cf7-85317fabaac7.html
Figure #1: Hanlon P, 2014, ‘Studies Support Massage Therapy for Preemies’,
Massage Magazine, Image courtesy of Getty Images, available at
https://www.massagemag.com/studies-support-massage-therapy-for-preemies-22584/
Figure #2: NICU App, 2011, ‘Neonatal Abstinence Syndrome’,
NICU App, available at
https://nicuapp.com/neonatal-abstinence-syndrome/
Figure #3: Nashville Medical News, 2019, ‘Benzodiazepine Use with Opioids Intensifies NAS’,
Nashville Medical News, available at
https://www.nashvillemedicalnews.com/article/2716/benzodiazepine-use-with-opioids-intensifies-nas
Figure #4: May B, 2019, ‘Incidence of Neonatal Abstinence Syndrome Has More Than Doubled’,
Neurology Advisor, available at
https://www.neurologyadvisor.com/topics/pediatric-neurology/incidence-of-neonatal-abstinence-syndrome-has-more-than-doubled/
Figure #5: NTMC, 2023, ‘Ongoing Recertification’,
Neonatal Touch & Massage Certification, available at
https://www.neonatalcertification.com/recertification/neonatal-touch-massage-recertification-ongoing/
Figure #6: Massage Magazine, 2017, ‘Reviewing the research on massage for preterm infants’, Massage Magazine, available at
https://www.massagemag.com/research-massage-preterm-infants-86675/
Play a crucial role in fostering the healthy development of infants, creating lasting bonds between parents and their babies.
The training was great! The trainer was so kind and patient. She was incredibly knowledgable and made the course very interesting. I'm looking forward to supporting parents and encouraging parent/child bonding. This is so beneficial for parents and babies, the more people who know about it, the better.
Paula answered all my queries and met all my expectations. The course was a good balance of theory & prac work.
I recently completed my 3 day face to face training. I Love, love, loved the trainer! This course exceeded my expectations. A lot was covered but it was presented sequentially and at a rate that you're able to digest. The power of doing the course face-to-face and networking with others was amazing. I was happy to hear there are future PD opportunities offered by IMIS and I will take advantage of these.
Our trainer was approachable and full of knowledge. The way she paced and structured the course was perfect. There was a good combination of theory and practical and I'm happy to recommend and endorse the course to others.
With my new Infant and Paediatric massage qualification, I'm looking forward to linking with services to support mothers with PND (community mental health services / inpatient and special units / services).

Very flexible, allowing you to complete the course on your own time. Overall, the course has been really interesting and I'm looking forward to commencing my adventure in teaching parents about baby massage.
Request a brochure